The death of a baby affects all parents differently but the grief is often overwhelming and prolonged. The intensity of love parents feel for their baby is not measurable in the weeks or months of pregnancy.

Miscarriage
Miscarriage is the spontaneous loss of a pregnancy before 24 weeks gestation. Miscarriage affects approximately 1 in 4 pregnancies.
Stillbirth
Stillbirth is the birth of a baby after 24 weeks gestation who did not show any signs of life after delivery. In the UK, 1 in 200 babies are born dead.
Livebirth
If there are any signs of life at delivery, at any gestation, this is a livebirth. If a liveborn baby subsequently dies, registration of both the birth and the death is required by law.
Termination for Fetal Abnormality
If following antenatal diagnosis there is substantial risk that if the child were born it would suffer from such physical or mental abnormalities as to be seriously handicapped women have the option of termination of pregnancy.
Communication with parents
The videos below may help you as a healthcare professional if you are involved in the care of parents who have experienced a stillbirth or neonatal death.
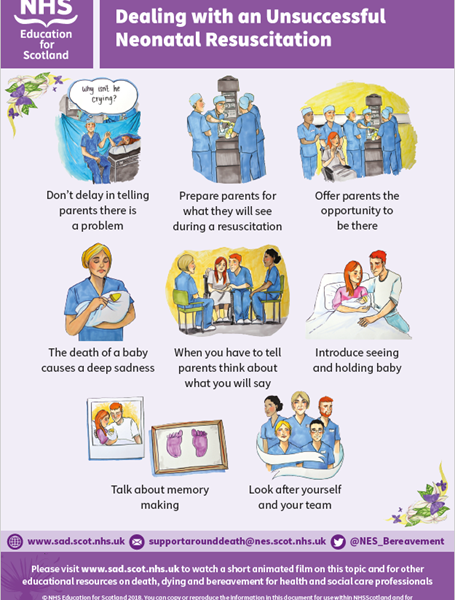
Dealing with unsuccessful neonatal resuscitation
Please note that this video deals with issues of death and bereavement and was created for healthcare professionals: caution is advised for viewers who are not healthcare professionals as some may find the themes upsetting.
A transcript of this video can be found here.
Downloadable poster: Dealing with an unsuccessful neonatal resuscitation - key messages
The Deafening Silence - Stillbirth through a Mother's Eyes
This film was created by Abigail's Footsteps as a tool for teaching those who work in maternity services about good and bad practice following a stillbirth or neonatal death.
Visit their website for more information.
Breaking the news of intrauterine death - animated video
Breaking the news of an intrauterine death is one of the most challenging parts of working within maternity settings. It can affect not only the patient but also the doctor and the wider team. This video aims to support healthcare professionals who work in maternity services and those who are involved in caring for patients who have experienced an intrauterine death.
A transcript of this video can be found here. A downloadable leaflet accompanying the video can be found here.
Postnatal care
After a baby has died, a mother will still experience the same physical and emotional postnatal reactions. Physical reminders of the loss, such as vaginal bleeding, the production of breastmilk, painful stitches or a caesarean scar may be very distressing. It is important to ensure that mothers have adequate pain relief and postnatal care.
Being with baby
Some parents will name their baby but some prefer not to. Be sensitive and ask what parents would prefer. Seeing and holding a baby after death can be frightening for parents. Some may not have seen a dead person before. Prepare them for what to expect. Many parents cherish this memory later.
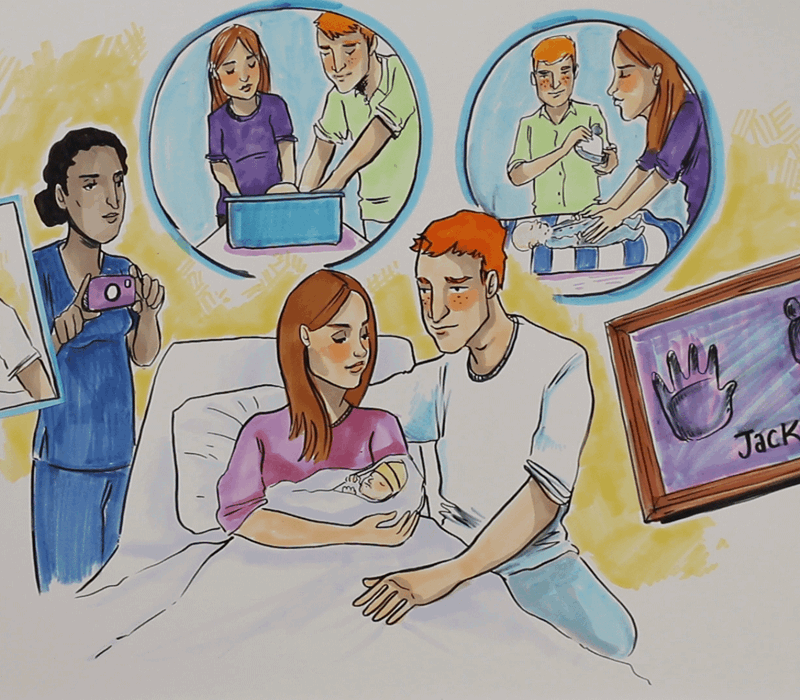
Memory making
Encourage parents whose baby has died to consider memory making. Parents may feel unsure about this but photos and keepsakes have been described by many as precious in the years to follow. The hospital bereavement team or maternity midwife may be able to help.
Some parents may find it difficult to decide whether to have photographs taken. However, bereaved parents have said that it’s better to have a photo that they may never look at rather than one they don’t have. If photos are taken on a mobile phone, remind parents to download them as soon as possible so that they are stored safely. Many parents value the opportunity to have photos of themselves caring (e.g. bathing or dressing) their baby, as well as photos of them holding their baby.
Many maternity departments in Scotland have digital cameras and memory boxes to help with memory making.
Termination of Pregnancy for Fetal Abnormality
Parents who make the decision to terminate their pregnancy following antenatal diagnosis of fetal abnormality will not only experience bereavement but also the guilt associated with their decision. It is important therefore that they receive the same level of care and support as any parent following the loss of their baby and should also be offered the same opportunities for memory making.
Multiple births
The loss of one twin or triplet can be very hard and confusing. Parents are grieving for the baby who has died but may also have ongoing concerns for the vulnerable survivor. Having a living baby does not reduce the grief for the baby or babies who have died and a living child’s progress can be a constant reminder of what might have been.
Deciding about a post mortem examination
If a baby dies after birth and the cause is unknown, the case must be referred to the Procurator Fiscal. Whilst this does not require parental authorisation, the reasons for this referral should be carefully explained to parents. Research shows that a post mortem examination may find new and often significant information about the cause of a baby’s death in 60-80% of cases. This may also discover whether there was a problem which could affect future pregnancies.
Post mortem examination can also contribute to important research into why babies die, and therefore potentially help to prevent more neonatal deaths in the future.
Deciding whether or not to have a post mortem can be an incredibly difficult decision to make. Some parents are desperate to know the reason why their baby died and others really may not want an examination.
Written information is available but remember to check reading ability and understanding. Allow time for parents to decide and ensure that regardless of the decision, parents know that their baby will be cared for at all times.
Types of post mortem examination
There are different types of post mortem: complete, limited or external only. It is important to go through the authorisation form carefully. Parents often have high expectations of a post mortem examination but sometimes there is no clear reason why a baby died. Even where a definitive cause of death is not identified, the examination can still yield useful information for families.
Results are usually available within 8 to 12 weeks but can take longer if specific tests are done on tissue samples. However, the funeral can take place once the main post mortem examination has been completed.
Parents should be offered an appointment to discuss the results of a post mortem examination.
Discussing Post Mortem Examination – film for healthcare professionals
This video aims to help healthcare professionals sensitively discuss authorised (hospital) post mortem examinations with families after a stillbirth or neonatal death.
Please note that this video deals with issues of death and bereavement and was created for healthcare professionals: caution is advised for viewers who are not healthcare professionals as some may find the themes upsetting.
A transcript of this video can be found here.
Parent to Parent Post Mortem Animation
This animated video was created by Held in Our Hearts.
This Parent to Parent Post Mortem Film draws on the experience of parents who have been bereaved, in order to comfort and inform others who face the decision of whether or not to proceed with a post mortem examination for their baby.
Please visit this page for more information on the video.
Supporting the professionals
Experiencing the loss of a baby within one’s capacity as a professional can also be very distressing. Ensure that you seek support from your colleagues and other sources. It is normal to think about this event for a long while after it has happened.
For the MBRRACE-UK Perinatal Mortality Surveillance Report - UK Perinatal Deaths for Births from January to December 2014, published in May 2016 click here
There are many sources of training and education for those who work with those who have experienced a pregnancy loss, stillbirth or neonatal death - search resources page. These include:
An e-learning module for those who work in maternity care services
Sands resources and training for professionals
Antenatal Results & Choices organisation Support and training for professionals
RCOG Good Practice document on registration of stillbirths and pregnancy loss before 24 weeks
Revised Guidance on the Disposal of Pregnancy Loss Up to and Including 23 Weeks and 6 Days Gestation, Scottish Government, April 2015
Infant Cremation Commission, Scottish Government, including Lord Bonomy report, 2014
The National Bereavement Care Pathway Scotland Project - Evidence-based care pathways designed for all healthcare professionals and staff who are involved in the care of women, partners and families at all stages of pregnancy and baby loss.
Practical support for parents
Coping with bereavement is a long process and there may be times of extreme distress and emotion. Getting back to daily routines can be very hard and parents often feel completely exhausted. Memories and anniversaries can bring back an overwhelming sense of loss. There are many available sources of advice and support, for example:
Stillbirth and Neonatal Death Society (Sands), information booklets online offering practical advice and support include
- When a baby dies before labour begins
- Saying goodbye to your baby
- Deciding about a post mortem: information for parents
- Mainly for fathers
- Going back to work after the death of your baby
- For family and friends: how you can help
- Supporting children when a baby has died
- Information and support for grandparents
- Information for employers: helping a bereaved parent return to work
- Another pregnancy: for parents whose baby has died
Bliss - Support and advice for families of babies in intensive care and special care, including bereaved families
Miscarriage association - Support and information for those affected by pregnancy loss
Twins and Multiple Birth Association (TAMBA) Bereavement Support Group - Support for families who have lost one or more children from a multiple birth
Scottish Care & Information on Miscarriage – Support for women and families in Scotland who have suffered miscarriage, stillbirth or neonatal loss
Held in Our Hearts - Provide support to families following the death of a baby through specialised bereavement services including befriending and counselling
Money Advice Service - Advice leaflet: Late miscarriage, stillbirth and neonatal death - A guide to the financial help available
Baby mailing preference service (MPS) - register online to stop or reduce baby related mailings
Antenatal Results & Choices (ARC) - Support for families affected by the diagnosis of fetal abnormality
One Milk Bank for Scotland - Milk bank hosted by NHS Greater Glasgow & Clyde, covering the whole of Scotland
Bereavement following a termination of pregnancy
It is important to note, that women who have had a termination of pregnancy, for whatever reason, may too experience feelings of grief. For more information on abortion, please visit NHS Inform.
Talking to parents about their decisions around burial or cremation after the death of their baby
This video includes guidance for professionals in Scotland on how to provide families who are bereaved with support and information about their options following the death of their baby. It will be of interest to a wide range of people, including healthcare professionals, funeral directors and crematoria staff.
A transcript of this video is available here.
For more information on discussing infant burial and cremation please click here